Addressing formulation challenges
New or additional formulations for drugs often need to be developed for a variety of reasons, such as to improve patient compliance (e.g., fewer doses, easier administration), reduce side effects, enhance drug stability, or increase bioavailability. During this process, common issues can include poor solubility, low permeability, and variable absorption, making predicting in vivo performance difficult.
A quantitative and efficient approach
This integrated PBPK and PBBM modeling approach provides a versatile solution applicable across all indications. By simulating the interplay between a drug’s formulation and human physiology, it enables the optimization of formulations with less reliance on extensive in vivo testing. This directly translates to accelerated development timelines and reduced costs, and our work advancing treatment for cryptococcal meningoencephalitis showcases the practical value of this methodology.
Real-world application
Advancing Cryptococcal Meningoencephalitis treatment
The mission was to guide critical decisions throughout the design and development of a new, easier-to-administer, and more patient-friendly sustained-release (SR) formulation of flucytosine: from formulation choice to understanding food effects, including disease effects on the drug pharmacokinetics (PK), to optimizing clinical trial design.
Background
The fungus cryptococcus neoformans is often found in soil and bird dropping and people are likely to breathe in this microscopic fungus at some point in their lives, but those with advanced HIV are particularly susceptible to infection due to their weakened immune system. The fungus can then invade the lining of the brain and other organs, which quickly leads to death unless treated.
When undiagnosed and untreated, the fungal infection is fatal.
With early diagnostic and optimal treatment, the survival rate is over 70%.
With the vast majority of infections and fatalities occurring in Africa, this alarming statistic points to a critical global health disparity, highlighting how socioeconomic factors intersect with neglected diseases to create profound challenges.
DNDi is a not-for-profit medical research organization that discovers, develops, and delivers safe, effective, and affordable treatments for neglected people. DNDi is developing medicines for sleeping sickness, leishmaniasis, Chagas disease, river blindness, mycetoma, dengue, paediatric HIV, advanced HIV disease, cryptococcal meningitis, and hepatitis C. Its research priorities include children’s health, gender equity and gender-responsive R&D, and diseases impacted by climate change. Since its creation in 2003, DNDi has joined with public and private partners across the globe to deliver 13 new treatments, saving millions of lives.
Flucytosine treatment
Flucytosine (5FC, or 5-Fluorocytosine) is a systemic antifungal medication in the antimetabolite agent class and a key, life-saving component of the World Health Organization (WHO)-recommended first- and second-line treatments for Cryptococcal Meningoencephalitis.
However, access to 5FC is not guaranteed in many countries where the infection is a frequent and serious health threat. Even where 5FC is available, it is challenging to use—the existing formulations of this vital drug present significant hurdles in the very settings where it is most needed.
The standard 5FC dosing regimen requires administration of four oral doses ― daily ― difficult to comply with in the often under-staffed and/or overburdened hospitals common in resource-limited environments.
Furthermore, as many patients may be admitted treatment in a state of coma, or at the very least, have problems swallowing, it is often crushed to be administered through nasogastric intubation – a pathway which the standard formulation was not designed for. This situation exemplifies how drug delivery, when not adapted to the realities, can exacerbate health inequities.
Recognizing these challenges, Drugs for Neglected Diseases initiative (DNDi) aimed to develop a simpler, sustained-release (SR) formulation of flucytosine (in addition to scaling up production and increasing accessibility for patients). A SR formulation is not only easier to administer – once or twice per day – but also better suited to the patients and constraints of the setting in which it is provided. By addressing these barriers, the project aims to bridge the gap between effective treatment and the socioeconomic realities faced by those most vulnerable to this deadly disease.
The planned clinical phase II trial of the sustained release pellet form of 5FC is as of February 2025 actively enrolling participants for administration of the investigational medicinal product. The trial aims to evaluate the pharmacokinetics, safety, tolerability, and preliminary efficacy in patients of this new formulation and marks a milestone of progress – significantly accelerated and made possible by a robust Model-Informed Drug Development (MIDD) strategy, specifically the application of Physiologically Based Pharmacokinetic (PBPK) modeling.
MIDD strategy and execution
Early model integration and iterative refinements, a core component of MIDD, facilitated informed decision-making throughout the drug development process.
Methodology
PBPK model development: An initial PBPK model was created based on limited literature data.
SR formulation design: The model was applied to guide SR prototype formulation development and dose selection.
Refinement & validation: The model was refined iteratively using data from two Phase 1 clinical studies with different flucytosine formulations under various prandial conditions in healthy participants.
Clinical application: The PBPK model was used to determine dosage for an upcoming Phase 2 clinical study with the selected sustained release formulation of 5FC, with a focus on low-weight patients.

Ad hoc simulations: The flexibility of MIDD allowed for quick assessments of ancillary questions, such as:
- Adding a loading dose for SR treatment.
- Assessing drug exposure in unconscious patients to refine therapeutic strategies.
Key findings
- Optimized dose selection: The PBPK model helped determine appropriate SR formulation doses for different patient populations, particularly low-weight individuals.
- Rapid decision-making: MIDD enabled fast and effective assessments of additional strategies to enhance treatment efficacy.
- Improved therapeutic outcomes: Model integration throughout the drug development process ensured adaptive, reliable decision-making, leading to a well-optimized SR flucytosine formulation.
Conclusion
This case study highlights the transformative potential of MIDD in accelerating drug development. PBPK modeling played a crucial role in optimizing the design and dosing of the SR formulation of flucytosine for CM treatment. The continuous integration of knowledge ensured model adaptability, demonstrating the effectiveness of MIDD in addressing evolving clinical challenges and improving patient outcomes.
Connected case studies
These additional case studies highlight individual components of the systematic model-informed drug development (MIDD) approach and center on the application of physiologically-based pharmacokinetic (PBPK) modeling and simulation to understand formulation performance.
The first study concentrated on the PBPK-informed design of sustained-release (SR) formulation prototypes. It established the required in vitro dissolution profile for an SR formulation to meet target pharmacokinetic (PK) profiles with twice-daily administration, using PBPK models developed primarily from literature data.
The second study built upon this by enabling the PBPK-informed selection of a specific SR formulation prototype and dosage for further clinical trials. This phase integrated initial clinical data to refine the models, supporting decisions that were presented to the World Health Organization (WHO).
The third study investigated the food effect on the PK profile of the selected SR formulation after transitioning from an immediate-release (IR) formulation. This analysis predicted how food intake might alter drug absorption and exposure, which informed patient recommendations and was also presented to the WHO.
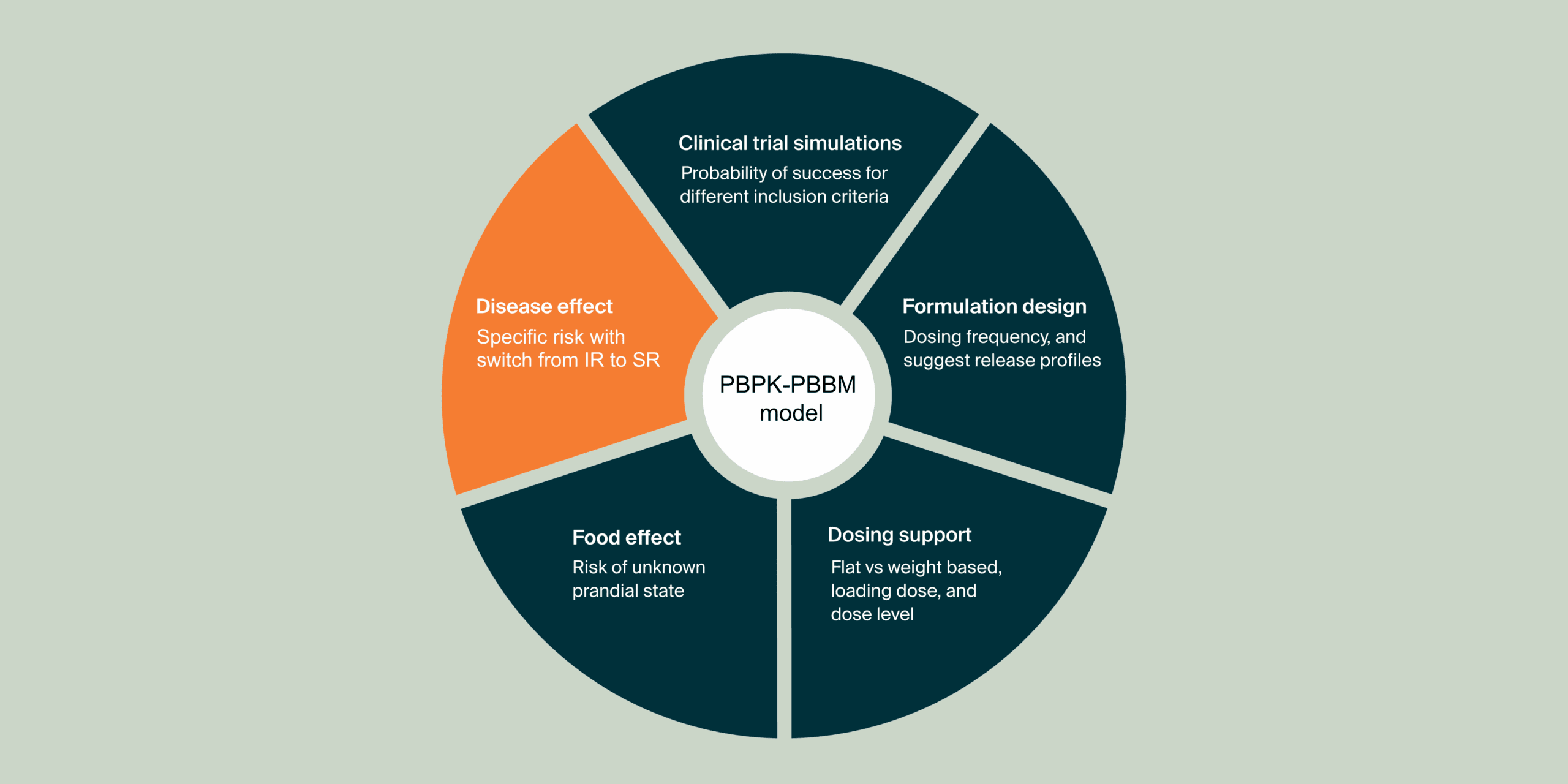
The fourth study investigated how the disease can impact flucytosine (5FC) PK profile after administration of a Sustained Release (SR) formulation in the context of a switch from an Immediate Release (IR) to a SR formulation for cryptococcal meningitis treatment in HIV patients. The results from this study supported the clinical phase 2 protocol design and the discussion with investigators.
Collectively, these excerpts illustrate a comprehensive MIDD strategy which integrate PBPK and PBBM modeling to guide the development of sustained-release formulations of flucytosine. The overarching objective is to achieve target drug concentrations with potentially less frequent dosing, ultimately aiming to improve patient outcomes in the treatment of cryptococcal meningitis in HIV-positive individuals.
Additional publications
Explore these publications focusing on specific parts of this project
Related posters & presentations
Read more or get in touch
Learn more about our PBPK-PBBM services